Key Takeaways
- The retinal pigment epithelium (RPE) is a single layer of pigmented cells that lies between the retina and the choroid in the eye.
- The RPE performs several vital functions that support the health and function of the retina, such as light absorption, epithelial transport, ion buffering, visual cycle, phagocytosis, secretion, and immune modulation.
- Dysfunction or damage of the RPE can lead to various retinal diseases, such as age-related macular degeneration, retinitis pigmentosa, diabetic retinopathy, albinism, and ocular melanosis.
Introduction
The eye is one of the most complex and fascinating organs in the human body. It allows us to perceive the world around us through vision, which is a process that involves many different structures and mechanisms. One of these structures is the retina, which is a thin layer of light-sensitive tissue that lines the back of the eye. The retina converts light into electrical signals that are transmitted to the brain via the optic nerve. The retina consists of several layers of cells, each with a specific role in vision. One of these layers is the retinal pigment epithelium (RPE), which is a single layer of pigmented cells that lies between the retina and the choroid (a layer of blood vessels that supplies oxygen and nutrients to the retina). The RPE performs several vital functions that support the health and function of the retina, such as light absorption, epithelial transport, ion buffering, visual cycle, phagocytosis, secretion, and immune modulation. In this article, we will explore what the RPE is, what it does, and what happens when it malfunctions.
What is the retina and how does it work?
The retina is a thin layer of light-sensitive tissue that lines the back of the eye. It consists of several layers of cells, including photoreceptors (rods and cones), bipolar cells, horizontal cells, amacrine cells, ganglion cells, and Müller cells. Photoreceptors are specialized cells that detect light and convert it into electrical signals. Rods are responsible for night vision and peripheral vision, while cones are responsible for color vision and central vision. Bipolar cells are intermediate cells that relay signals from photoreceptors to ganglion cells. Horizontal cells and amacrine cells are interneurons that modulate signals between photoreceptors and bipolar cells. Ganglion cells are output neurons that transmit signals from bipolar cells to the optic nerve. Müller cells are glial cells that provide structural and metabolic support to other retinal cells.
The retina works by capturing light rays that enter the eye through the pupil (the opening in the center of the iris) and pass through the lens (a transparent structure that focuses light onto the retina). The light rays then hit the photoreceptors in the outermost layer of the retina. The photoreceptors contain light-sensitive molecules called opsins, which change their shape when they absorb light. This triggers a cascade of chemical reactions that generate electrical signals in the photoreceptors. These signals are then passed on to bipolar cells, which in turn pass them on to ganglion cells. The ganglion cells then send their signals along their axons (long extensions) that form the optic nerve. The optic nerve carries these signals to the brain, where they are processed by various regions to form visual images.
What is the retinal pigment epithelium and what are its functions?
The retinal pigment epithelium (RPE) is a single layer of pigmented cells that lies between the retina and the choroid in the eye. The RPE is composed of hexagonal cells that are densely packed with pigment granules called melanosomes. The RPE cells are connected by tight junctions that form a barrier between the retina and the choroid. The RPE cells also have microvilli (small projections) that extend into the space between the photoreceptors and the RPE. The RPE performs several vital functions that support the health and function of the retina, such as:
- Light absorption and protection: The RPE absorbs excess light that reaches the retina and prevents it from reflecting back and causing glare. The pigment granules in the RPE also protect the retina from harmful ultraviolet (UV) radiation and oxidative stress.
- Epithelial transport and blood-retinal barrier: The RPE regulates the exchange of substances between the retina and the choroid. The RPE transports nutrients, oxygen, water, ions, and metabolites from the choroid to the retina, and removes waste products, carbon dioxide, and water from the retina to the choroid. The RPE also forms part of the blood-retinal barrier, which prevents the leakage of blood components and pathogens into the retina.
- Spatial buffering of ions and pH regulation: The RPE maintains the ionic balance and pH of the subretinal space (the space between the photoreceptors and the RPE). The RPE pumps out excess potassium ions that accumulate in the subretinal space due to phototransduction (the process of converting light into electrical signals). The RPE also regulates the pH of the subretinal space by secreting bicarbonate ions and absorbing hydrogen ions.
- Visual cycle and retinoid metabolism: The RPE participates in the visual cycle, which is a series of chemical reactions that regenerate the light-sensitive molecules in the photoreceptors. The RPE converts all-trans-retinal (a form of vitamin A that is released from opsins after light absorption) into 11-cis-retinal (a form of vitamin A that binds to opsins to form functional photopigments). The RPE also stores excess vitamin A in lipid droplets called retinyl esters.
- Phagocytosis and recycling of photoreceptor outer segments: The RPE phagocytoses (engulfs and digests) the shed tips of photoreceptor outer segments (POS), which are constantly renewed by photoreceptors. The RPE recycles some of the components of POS, such as fatty acids, cholesterol, proteins, and retinoids, and discards others as waste products.
- Secretion and immune modulation: The RPE secretes various factors that influence the development, survival, differentiation, and function of retinal cells. Some of these factors include growth factors, cytokines, neurotrophins, antioxidants, and extracellular matrix proteins. The RPE also modulates the immune response in the eye by expressing immunosuppressive molecules and presenting antigens to immune cells.
Functions of the Retinal Pigment Epithelium
Light absorption and protection
One of the main functions of the RPE is to absorb excess light that reaches the retina and prevent it from reflecting back and causing glare. This improves the contrast and clarity of vision. The pigment granules in the RPE contain melanin, a dark brown pigment that absorbs light. Melanin also protects the retina from harmful ultraviolet (UV) radiation and oxidative stress. UV radiation can damage DNA, proteins, lipids, and other molecules in retinal cells, leading to cell death or mutation. Oxidative stress is caused by reactive oxygen species (ROS), which are unstable molecules that can react with and damage other molecules. ROS are generated by various sources, such as UV radiation, inflammation, metabolism, or environmental toxins. The RPE has a high capacity to scavenge ROS by producing antioxidants, such as glutathione, vitamin C, vitamin E, catalase, superoxide dismutase, and glutathione peroxidase.
Epithelial transport and blood-retinal barrier
Another important function of the RPE is to regulate the exchange of substances between the retina and the choroid. The retina has a high metabolic demand and requires a constant supply of nutrients, oxygen, water, ions, and metabolites from the choroid. The retina also produces waste products, carbon dioxide, and water that need to be removed to the choroid. The RPE transports these substances across its cell membrane by using various transporters, channels, pumps, receptors, and enzymes. For example, the RPE transports glucose (a major source of energy for retinal cells) from the choroid to the retina by using glucose transporters (GLUTs). The RPE also transports lactate (a product of anaerobic glycolysis) from the retina to the choroid by using monocarboxylate transporters (MCTs). The RPE also transports water from the retina to the choroid by using aquaporins (AQPs), which are water channels. The RPE also transports ions, such as sodium, potassium, calcium, chloride, and bicarbonate, from the choroid to the retina or vice versa by using various ion channels, pumps, and exchangers. For example, the RPE transports sodium from the choroid to the retina by using sodium-potassium ATPase (Na+/K±ATPase), which is a pump that uses energy from ATP to move sodium and potassium ions across the membrane. The RPE also transports calcium from the retina to the choroid by using calcium-ATPase (Ca2±ATPase), which is another pump that uses energy from ATP to move calcium ions across the membrane.
The RPE also forms part of the blood-retinal barrier, which is a physical and functional barrier that prevents the leakage of blood components and pathogens into the retina. The blood-retinal barrier consists of two components: the inner blood-retinal barrier and the outer blood-retinal barrier. The inner blood-retinal barrier is formed by the tight junctions between the endothelial cells of the retinal capillaries, which are the smallest blood vessels in the retina. The outer blood-retinal barrier is formed by the tight junctions between the RPE cells, which seal the space between the retina and the choroid. The tight junctions are composed of various proteins, such as occludin, claudin, zonula occludens, and junctional adhesion molecules, that link the membranes of adjacent cells and prevent the passage of molecules and ions between them. The blood-retinal barrier protects the retina from harmful substances, such as toxins, drugs, antibodies, or microbes, that may enter the bloodstream. The blood-retinal barrier also maintains the homeostasis of the retina by regulating the concentration of substances in the subretinal space.
Spatial buffering of ions and pH regulation
Another crucial function of the RPE is to maintain the ionic balance and pH of the subretinal space. The subretinal space is the space between the photoreceptors and the RPE. The subretinal space contains a fluid called subretinal fluid (SRF), which is derived from plasma (the liquid part of blood) and vitreous humor (a gel-like substance that fills the eye). The SRF provides a medium for light transmission and diffusion of substances between the retina and the RPE. The SRF also contains various ions, such as potassium, sodium, calcium, chloride, and bicarbonate, that are essential for phototransduction and cell function.
The RPE maintains the ionic balance and pH of the subretinal space by pumping out excess potassium ions that accumulate in the subretinal space due to phototransduction. Phototransduction is the process of converting light into electrical signals in photoreceptors. Phototransduction involves a series of events that lead to changes in membrane potential and ion fluxes in photoreceptors. When light hits a photoreceptor, it activates an opsin, which in turn activates a G protein called transducin. Transducin then activates a phosphodiesterase (PDE), which breaks down cyclic guanosine monophosphate (cGMP), a second messenger that regulates ion channels. As cGMP levels decrease, sodium channels close and potassium channels open in photoreceptors. This causes an influx of potassium ions into photoreceptors and an efflux of potassium ions into the subretinal space. As a result, the subretinal space becomes hyperpolarized (more negative) and hyperkalemic (high in potassium) compared to the choroid. This creates an electrical gradient and an osmotic gradient across the RPE.
The RPE responds to these gradients by pumping out potassium ions from the subretinal space to the choroid by using Na+/K±ATPase and other potassium transporters. This restores the normal membrane potential and osmolarity of the subretinal space. The RPE also regulates the pH of the subretinal space by secreting bicarbonate ions and absorbing hydrogen ions. Bicarbonate ions are produced by carbonic anhydrase (CA), an enzyme that catalyzes the reaction between carbon dioxide and water. Hydrogen ions are generated by various metabolic processes in retinal cells. The RPE uses bicarbonate transporters (such as NBCs) and chloride-bicarbonate exchangers (such as AE2) to move bicarbonate ions across its membrane. The RPE also uses proton pumps (such as V-ATPase) and sodium-hydrogen exchangers (such as NHEs) to move hydrogen ions across its membrane. By doing so, the RPE maintains the pH of the subretinal space at around 7.4, which is optimal for phototransduction and cell function.
Visual cycle and retinoid metabolism
Another vital function of the RPE is to participate in the visual cycle, which is a series of chemical reactions that regenerate the light-sensitive molecules in photoreceptors. The light-sensitive molecules in photoreceptors are called photopigments, which consist of an opsin (a protein) and a chromophore (a light-absorbing molecule). The chromophore in rods is called rhodopsin, while the chromophores in cones are called cone opsins. The chromophores are derived from vitamin A, which is a fat-soluble vitamin that is obtained from the diet or synthesized from beta-carotene (a plant pigment). Vitamin A exists in different forms, such as retinol (alcohol form), retinal (aldehyde form), and retinoic acid (acid form). The most important form for vision is retinal, which binds to opsins to form functional photopigments.
The visual cycle involves the conversion of retinal between two isomeric forms: 11-cis-retinal and all-trans-retinal. 11-cis-retinal is the form that binds to opsins to form functional photopigments. All-trans-retinal is the form that is released from opsins after light absorption. The visual cycle regenerates 11-cis-retinal from all-trans-retinal, so that it can bind to opsins again and restore the sensitivity of photoreceptors. The visual cycle occurs in both photoreceptors and the RPE, but the RPE plays a major role in this process.
The visual cycle starts in photoreceptors, where light hits a photopigment and activates it. This causes a conformational change in the opsin and the chromophore, leading to the release of all-trans-retinal from the opsin. The all-trans-retinal then undergoes a series of reactions that reduce it to all-trans-retinol (a form of vitamin A that can cross membranes). The all-trans-retinol then diffuses out of photoreceptors and into the subretinal space, where it binds to a carrier protein called interphotoreceptor retinoid-binding protein (IRBP). IRBP transports the all-trans-retinol to the RPE, where it is taken up by RPE cells.
The RPE then continues the visual cycle by converting the all-trans-retinol into 11-cis-retinal. The RPE does this by using various enzymes, such as lecithin-retinol acyltransferase (LRAT), retinyl ester hydrolase (REH), retinol dehydrogenase (RDH), retinal dehydrogenase (RALDH), and RPE65. LRAT esterifies (adds a fatty acid) to all-trans-retinol to form all-trans-retinyl ester, which is stored in lipid droplets in RPE cells. REH hydrolyzes (removes a fatty acid) from all-trans-retinyl ester to release all-trans-retinol, which is then oxidized (loses electrons) by RDH to form all-trans-retinal. All-trans-retinal is then isomerized (changes its shape) by RALDH and RPE65 to form 11-cis-retinal. 11-cis-retinal then diffuses out of RPE cells and into the subretinal space, where it binds to IRBP again. IRBP transports the 11-cis-retinal back to photoreceptors, where it binds to opsins to form functional photopigments. This completes the visual cycle and restores the sensitivity of photoreceptors.
Phagocytosis and recycling of photoreceptor outer segments
Another essential function of the RPE is to phagocytose (engulf and digest) the shed tips of photoreceptor outer segments (POS), which are constantly renewed by photoreceptors. Photoreceptors have two segments: an inner segment and an outer segment. The inner segment contains the nucleus and other organelles, while the outer segment contains stacks of membranous discs that contain photopigments. The outer segment is constantly exposed to light and oxidative stress, which damage its discs and impair its function. To cope with this damage, photoreceptors continuously synthesize new discs at the base of their outer segment and shed old discs at the tip of their outer segment. The shed discs are then phagocytosed by the RPE, which recycles some of their components and discards others as waste products.
The phagocytosis of POS by the RPE is a complex and regulated process that involves several steps, such as recognition, binding, internalization, degradation, and recycling. The recognition of POS by the RPE is mediated by various receptors, such as integrins, CD36, αvβ5, and MerTK, that bind to specific ligands, such as phosphatidylserine, vitronectin, and Gas6, that are exposed on the surface of POS. The binding of POS to RPE receptors triggers the activation of various signaling pathways, such as FAK, PI3K/Akt, and MAPK, that regulate the cytoskeleton and membrane dynamics of RPE cells. The internalization of POS by the RPE is achieved by the formation of phagosomes (membrane-bound vesicles) that engulf POS and fuse with lysosomes (organelles that contain digestive enzymes) to form phagolysosomes. The degradation of POS by the RPE is accomplished by the action of various hydrolases (enzymes that break down molecules) that are present in lysosomes, such as cathepsins, lipases, proteases, and nucleases. The recycling of POS by the RPE is performed by the reuse or export of some of the components of POS, such as fatty acids, cholesterol, proteins, and retinoids. The RPE also discards some of the components of POS as waste products, such as melanin granules and lipofuscin (a brownish pigment that accumulates in RPE cells).
The phagocytosis of POS by the RPE is essential for the maintenance and function of photoreceptors. The phagocytosis of POS removes damaged discs and prevents their accumulation in the subretinal space, which could impair light transmission and cause inflammation. The phagocytosis of POS also provides a source of nutrients and retinoids for the RPE and photoreceptors. The phagocytosis of POS also modulates the gene expression and secretion of various factors by the RPE that influence the development, survival, differentiation, and function of retinal cells.
Secretion and immune modulation
Another important function of the RPE is to secrete various factors that influence the development, survival, differentiation, and function of retinal cells. Some of these factors include growth factors, cytokines, neurotrophins, antioxidants, and extracellular matrix proteins. Growth factors are molecules that stimulate cell growth, proliferation, differentiation, migration, or survival. Some examples of growth factors secreted by the RPE are vascular endothelial growth factor (VEGF), pigment epithelium-derived factor (PEDF), fibroblast growth factor (FGF), transforming growth factor beta (TGF-β), insulin-like growth factor (IGF), and epidermal growth factor (EGF). Cytokines are molecules that regulate inflammation and immunity. Some examples of cytokines secreted by the RPE are interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10), tumor necrosis factor alpha (TNF-α), and interferon gamma (IFN-γ). Neurotrophins are molecules that support the survival and function of neurons. Some examples of neurotrophins secreted by the RPE are brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), neurotrophin-3 (NT-3), and neurotrophin-4/5 (NT-4/5). Antioxidants are molecules that protect cells from oxidative stress. Some examples of antioxidants secreted by the RPE are glutathione, vitamin C, vitamin E, catalase, superoxide dismutase, and glutathione peroxidase. Extracellular matrix proteins are molecules that provide structural and functional support to cells. Some examples of extracellular matrix proteins secreted by the RPE are collagen, laminin, fibronectin, and elastin.
The secretion of these factors by the RPE has various effects on retinal cells. For example, VEGF stimulates the formation of new blood vessels in the retina, PEDF inhibits angiogenesis (blood vessel formation) and promotes neuronal survival in the retina, FGF promotes photoreceptor differentiation and survival in the retina, TGF-β regulates cell proliferation and differentiation in the retina, IGF enhances photoreceptor survival and function in the retina, EGF stimulates cell proliferation and migration in the retina, IL-1 induces inflammation and apoptosis (cell death) in the retina, IL-6 regulates immune responses and wound healing in the retina, IL-8 attracts immune cells to the retina, IL-10 suppresses inflammation and immune responses in the retina, TNF-α induces inflammation and apoptosis in the retina, IFN-γ activates immune cells and inhibits viral infections in the retina, BDNF protects photoreceptors and ganglion cells from degeneration in the retina, NGF supports the survival and function of ganglion cells in the retina, NT-3 promotes the survival and differentiation of photoreceptors and bipolar cells in the retina, NT-4/5 protects photoreceptors from light-induced damage in the retina, glutathione scavenges ROS and detoxifies xenobiotics (foreign substances) in the retina, vitamin C reduces oxidative stress and regenerates vitamin E in the retina, vitamin E protects cell membranes from lipid peroxidation (oxidative damage) in the retina, catalase decomposes hydrogen peroxide (a ROS) into water and oxygen in the retina, superoxide dismutase converts superoxide (a ROS) into hydrogen peroxide and oxygen in the retina, glutathione peroxidase reduces hydrogen peroxide and lipid hydroperoxides (oxidized lipids) into water and alcohols in the retina, collagen provides strength and elasticity to the retina, laminin promotes cell adhesion and differentiation in the retina, fibronectin facilitates cell migration and wound healing in the retina, and elastin provides flexibility and resilience to the retina.
Another significant function of the RPE is to modulate the immune response in the eye by expressing immunosuppressive molecules and presenting antigens to immune cells. The eye is an immune privileged site, which means that it has a reduced or altered immune response to prevent inflammation and damage to its delicate structures. The RPE contributes to the immune privilege of the eye by expressing various molecules that suppress or regulate the activation, proliferation, differentiation, or function of immune cells, such as T cells, B cells, macrophages, dendritic cells, natural killer cells, or mast cells. Some of these molecules include Fas ligand (FasL), programmed death ligand 1 (PD-L1), transforming growth factor beta (TGF-β), interleukin-10 (IL-10), indoleamine 2,3-dioxygenase (IDO), prostaglandin E2 (PGE2), and complement regulatory proteins (CRPs). The RPE also presents antigens (molecules that trigger an immune response) to immune cells by using major histocompatibility complex (MHC) molecules, which are proteins that bind to antigens and display them on the cell surface. The RPE expresses both MHC class I and MHC class II molecules, which present antigens to different types of T cells. MHC class I molecules present antigens to cytotoxic T cells, which kill infected or abnormal cells. MHC class II molecules present antigens to helper T cells, which coordinate the immune response by secreting cytokines. The RPE also expresses co-stimulatory molecules, such as CD80, CD86, and CD40, which are proteins that enhance or inhibit the activation of T cells by binding to their receptors, such as CD28, CTLA-4, and CD40L.
The modulation of the immune response by the RPE has various effects on the eye. For example, FasL induces apoptosis of activated T cells that infiltrate the eye, PD-L1 inhibits the activation and function of T cells that recognize antigens presented by RPE cells, TGF-β induces the differentiation of regulatory T cells (Tregs), which suppress inflammation and autoimmunity in the eye, IL-10 inhibits the production of pro-inflammatory cytokines and enhances the production of anti-inflammatory cytokines in the eye, IDO degrades tryptophan (an essential amino acid) into kynurenine (a metabolite), which inhibits the proliferation and function of T cells and induces the differentiation of Tregs in the eye, PGE2 inhibits the production of pro-inflammatory cytokines and enhances the production of anti-inflammatory cytokines in the eye, CRPs prevent the activation of complement system (a part of innate immunity) that can cause inflammation and tissue damage in the eye, MHC class I molecules present antigens to cytotoxic T cells that eliminate virus-infected or tumor cells in the eye, MHC class II molecules present antigens to helper T cells that activate adaptive immunity (a part of specific immunity) against pathogens or foreign substances in the eye, and co-stimulatory molecules fine-tune the activation or inhibition of T cells depending on the context and signals in the eye.
Diseases of the Retinal Pigment Epithelium
The RPE is essential for the health and function of the retina, but it can also be affected by various diseases that impair its structure or function. Some of these diseases are:
- Age-related macular degeneration (AMD): AMD is a degenerative disease that affects the macula, which is the central part of the retina that is responsible for high-resolution and color vision. AMD causes the loss of central vision and the distortion of images. AMD is classified into two types: dry AMD and wet AMD. Dry AMD is characterized by the accumulation of drusen (yellowish deposits) and the atrophy (wasting away) of the RPE and photoreceptors in the macula. Wet AMD is characterized by the growth of abnormal blood vessels from the choroid into the retina, which leak fluid and blood and cause scarring and damage to the RPE and photoreceptors in the macula. The exact causes of AMD are not fully understood, but some risk factors include aging, genetics, smoking, obesity, hypertension, and exposure to sunlight. There is no cure for AMD, but some treatments can slow down its progression or improve its symptoms, such as antioxidant supplements, anti-VEGF injections, laser therapy, or photodynamic therapy.
- Retinitis pigmentosa (RP): RP is a group of inherited diseases that affect the photoreceptors in the retina. RP causes the progressive loss of night vision, peripheral vision, and color vision. RP is caused by mutations in various genes that encode proteins involved in phototransduction, visual cycle, or photoreceptor development or maintenance. Some examples of these genes are RHO, RPE65, ABCA4, and RPGR. The mutations lead to the dysfunction or death of photoreceptors and the formation of bone spicules (pigment clumps) in the retina. The RPE is also affected by RP, as it has to cope with increased oxidative stress, impaired visual cycle, and reduced phagocytosis of POS. There is no cure for RP, but some treatments can slow down its progression or improve its symptoms, such as vitamin A supplements, retinal implants, gene therapy, or stem cell therapy.
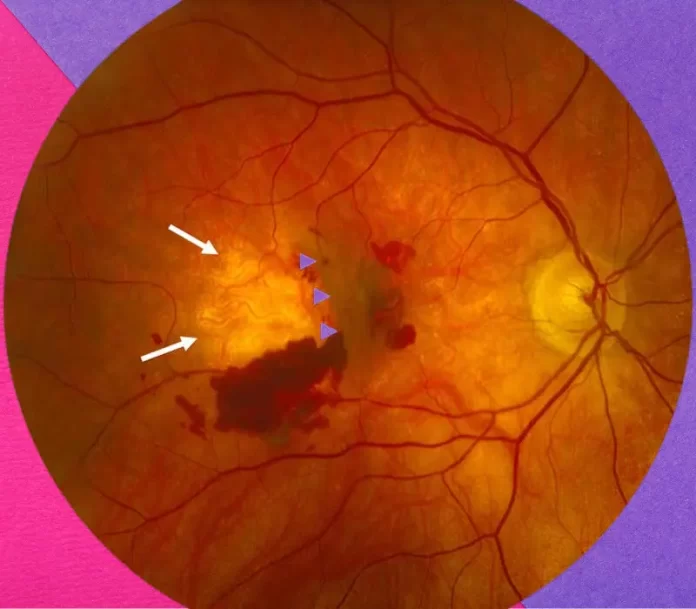
- Diabetic retinopathy (DR): DR is a complication of diabetes mellitus (a metabolic disorder that causes high blood sugar levels) that affects the retina. DR causes the damage or leakage of blood vessels in the retina, which leads to edema (swelling), hemorrhage (bleeding), ischemia (lack of oxygen), or neovascularization (new blood vessel formation). DR can cause blurred vision, floaters (spots or lines in vision), or blindness. DR is classified into two stages: non-proliferative DR and proliferative DR. Non-proliferative DR is characterized by microaneurysms (ballooning of blood vessels), dot-and-blot hemorrhages (small spots of bleeding), hard exudates (deposits of lipids or proteins), and macular edema (swelling of the macula). Proliferative DR is characterized by neovascularization of the retina or the optic disc (the point where the optic nerve exits the eye), vitreous hemorrhage (bleeding into the vitreous humor), or tractional retinal detachment (pulling away of the retina from the RPE due to scar tissue). The RPE is also affected by DR, as it has to cope with increased oxidative stress, impaired epithelial transport, disrupted blood-retinal barrier, or altered secretion of factors. The main causes of DR are hyperglycemia (high blood sugar levels), hypertension (high blood pressure), dyslipidemia (abnormal levels of lipids in blood), or inflammation. The main treatments for DR are glycemic control (keeping blood sugar levels within normal range), blood pressure control, lipid-lowering drugs, laser photocoagulation (burning abnormal blood vessels with laser), anti-VEGF injections, or vitrectomy (removal of vitreous humor).
- Albinism and ocular melanosis: Albinism and ocular melanosis are two opposite conditions that affect the pigmentation of the RPE and other ocular structures. Albinism is a genetic disorder that causes a deficiency or absence of melanin in the RPE and other ocular structures, such as iris, choroid, and optic nerve. Albinism causes reduced visual acuity (sharpness of vision), nystagmus (involuntary eye movements), strabismus (misalignment of eyes), photophobia (sensitivity to light), or hypopigmentation (lightening of skin or hair color). Albinism is caused by mutations in various genes that encode enzymes involved in melanin synthesis, such as tyrosinase (TYR), oculocutaneous albinism type 2 (OCA2), tyrosinase-related protein 1 (TYRP1), or solute carrier family 45 member 2 (SLC45A2). Ocular melanosis is a rare disorder that causes an excess of melanin in the RPE and other ocular structures, such as iris, choroid, and sclera (the white part of the eye). Ocular melanosis causes increased pigmentation (darkening of skin or eye color), glaucoma (increased pressure in the eye), or uveal melanoma (a type of eye cancer). Ocular melanosis is caused by mutations in the GNAQ or GNA11 genes, which encode proteins involved in signaling pathways that regulate cell growth and differentiation. There is no cure for albinism or ocular melanosis, but some treatments can improve their symptoms, such as glasses, contact lenses, sunglasses, eye drops, or surgery.
Conclusion
The retinal pigment epithelium (RPE) is a single layer of pigmented cells that lies between the retina and the choroid in the eye. The RPE performs several vital functions that support the health and function of the retina, such as light absorption, epithelial transport, ion buffering, visual cycle, phagocytosis, secretion, and immune modulation. Dysfunction or damage of the RPE can lead to various retinal diseases, such as age-related macular degeneration, retinitis pigmentosa, diabetic retinopathy, albinism, and ocular melanosis. The RPE is a remarkable and versatile tissue that plays a key role in vision and ocular health.
FAQs
What is the difference between the RPE and the choroid?
The RPE is a single layer of pigmented cells that lies between the retina and the choroid in the eye. The choroid is a layer of blood vessels that lies between the RPE and the sclera in the eye. The RPE regulates the exchange of substances between the retina and the choroid, while the choroid provides oxygen and nutrients to the retina and the RPE.
How does the RPE absorb light and protect the retina from UV radiation and oxidative stress?
The RPE absorbs light by using pigment granules called melanosomes that contain melanin, a dark brown pigment that absorbs light. The RPE protects the retina from UV radiation and oxidative stress by using melanin and antioxidants. Melanin blocks harmful UV rays from reaching the retina and causing DNA damage. Antioxidants scavenge reactive oxygen species (ROS) that are generated by UV radiation or other sources and cause oxidative damage to molecules in retinal cells.
How does the RPE participate in the visual cycle and regenerate the light-sensitive molecules in photoreceptors?
The RPE participates in the visual cycle by converting all-trans-retinal (a form of vitamin A that is released from opsins after light absorption) into 11-cis-retinal (a form of vitamin A that binds to opsins to form functional photopigments). The RPE does this by using various enzymes, such as lecithin-retinol acyltransferase (LRAT), retinyl ester hydrolase (REH), retinol dehydrogenase (RDH), retinal dehydrogenase (RALDH), and RPE65. The RPE also stores excess vitamin A in lipid droplets called retinyl esters.
How does the RPE phagocytose and recycle the shed tips of photoreceptor outer segments (POS)?
The RPE phagocytoses POS by using various receptors, such as integrins, CD36, αvβ5, and MerTK, that bind to specific ligands on POS. The RPE then forms phagosomes that engulf POS and fuse with lysosomes to form phagolysosomes. The RPE then degrades POS by using various hydrolases that are present in lysosomes. The RPE recycles some of the components of POS, such as fatty acids, cholesterol, proteins, and retinoids, and discards others as waste products, such as melanin granules and lipofuscin.
How does the RPE secrete various factors that influence the development, survival, differentiation, and function of retinal cells?
The RPE secretes various factors by using various mechanisms, such as exocytosis (release of vesicles containing factors), transcytosis (transport of factors across cells), or paracrine signaling (release of factors into extracellular space). Some examples of factors secreted by the RPE are growth factors, cytokines, neurotrophins, antioxidants, and extracellular matrix proteins. These factors have various effects on retinal cells, such as stimulating cell growth, proliferation, differentiation, migration, or survival, regulating inflammation and immunity, supporting neuronal survival and function, protecting cells from oxidative stress, and providing structural and functional support to cells.